Tibialis Anterior Tendinopathy and Rupture
What and where is Tibialis Anterior?
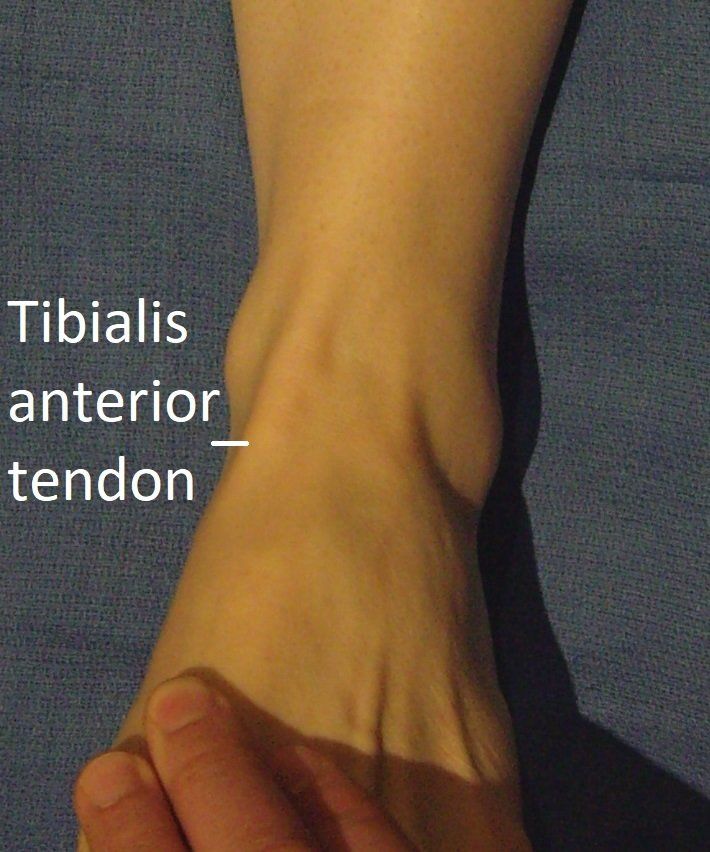
Tibialis anterior is the largest shin muscle. Its tendon runs down the front of the ankle to connect with the inner side of the foot.
This is the third largest ankle tendon
(after the Achilles and tibialis posterior). It pulls the foot up when walking, allowing the foot to clear the ground, and also supports the medial arch.
What can go wrong with Tibialis Anterior?
Like all tendons, tibialis anterior can become "inflamed" by overuse and "worn" by aging.
This can cause:
- reactive "tendinitis"
- degenerative tendinopathy and split tears
- complete rupture.
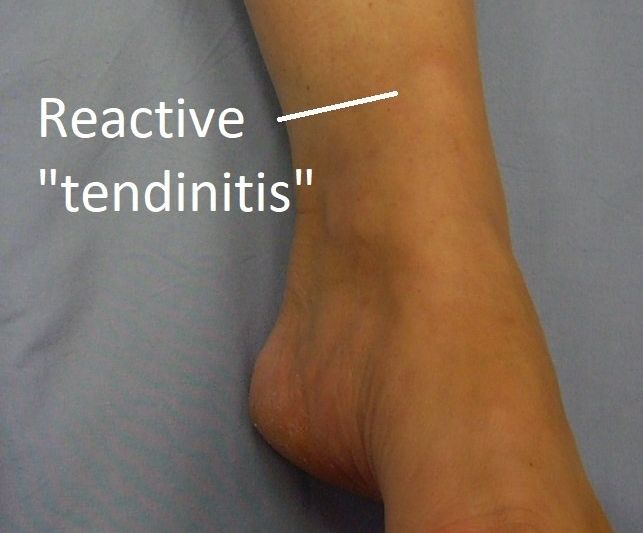
Tibialis Anterior Reactive "Tendinitis"
This is a cause of anterior ankle pain
and swelling in hill runners. It is due to overuse (increased intensity and/or duration).
Non-operative treatment (rest, anti-inflammatory medication and cortisone injections) settle most people.
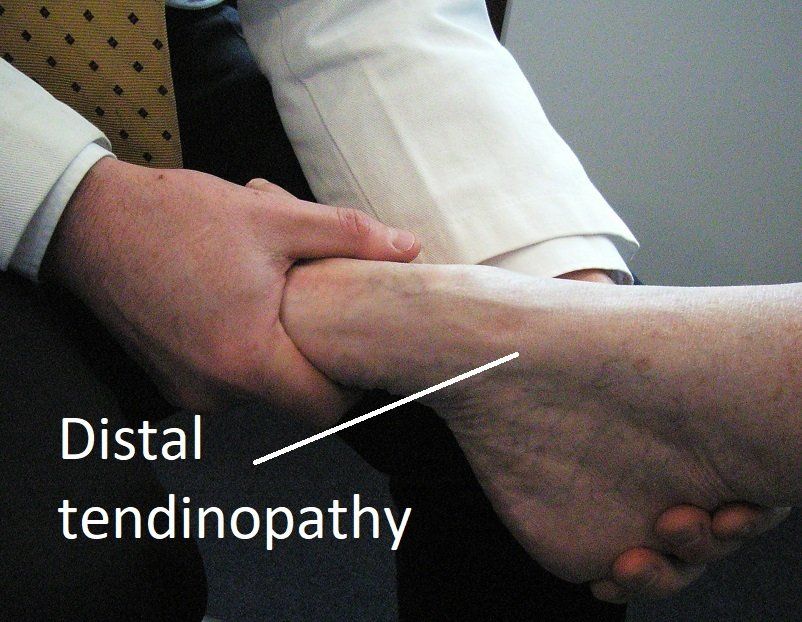
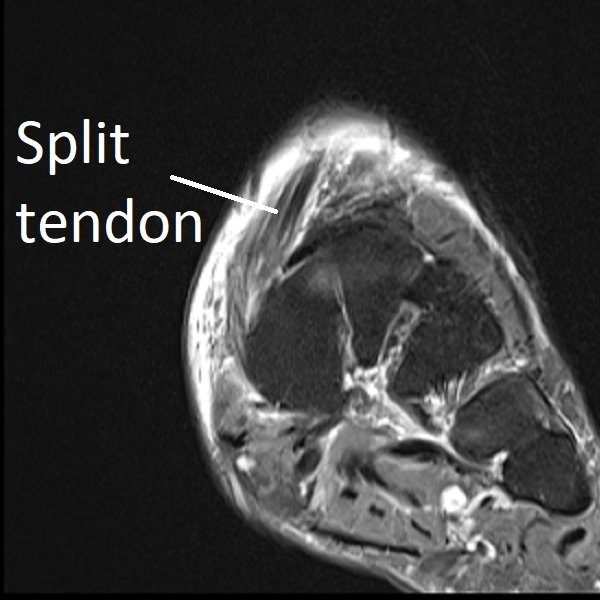
Tibialis Anterior Tendinopathy and Split Tears
Over time, "wear and tear" can accumulate in the tibialis anterior tendon. This is usually in the last (distal) 4 cm of the tendon.
It is more common in women, people aged over 60, those with midfoot arthritis, and who are over-weight.
Symptoms are in the medial (inner) midfoot
and arch, and include:
- activity-related pain
- night-time burning pain
- swelling.
Occasionally, this part of the tendon can split. Pain and swelling usually become more severe.
Interesting fact: Dr Beamond studied this condition in Melbourne during 2007/2008, and published the first paper on it in 2009.
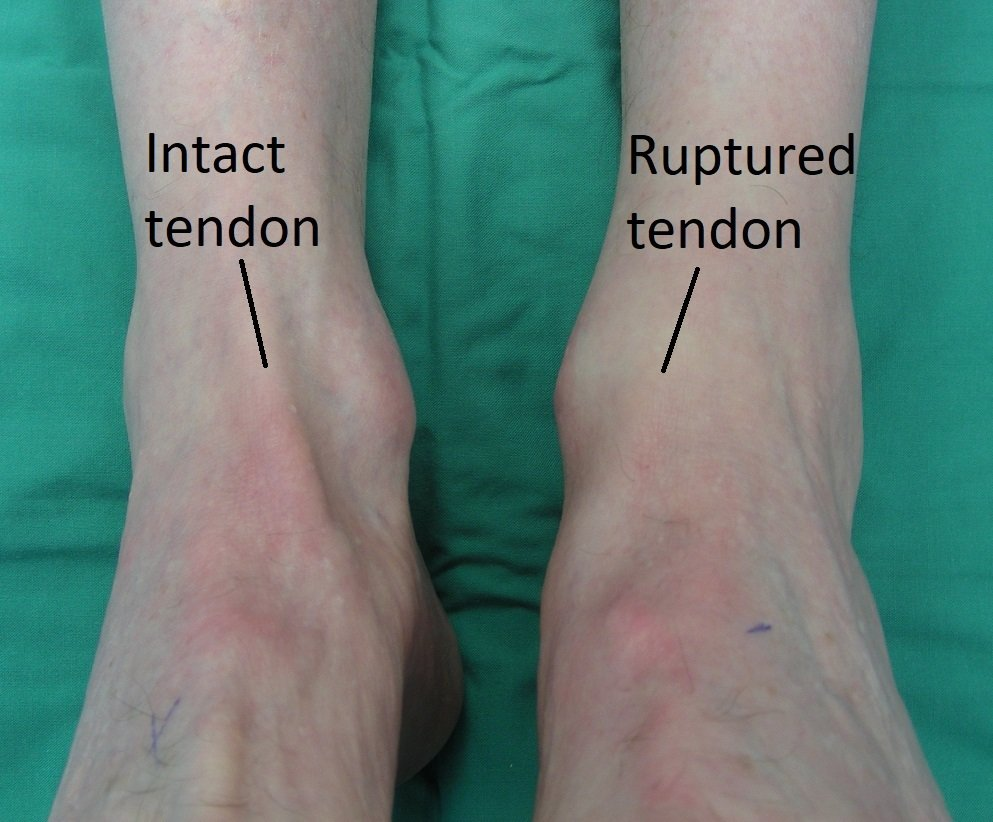
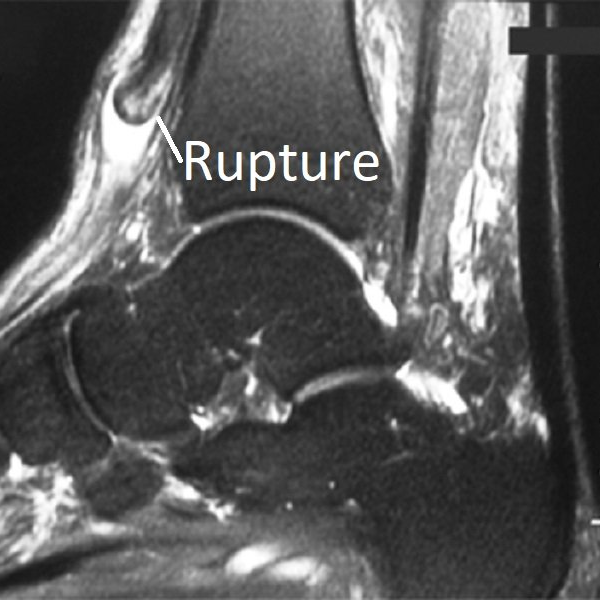
Tibialis Anterior Complete Rupture
Like the Achilles tendon
and peroneal tendons, the tendon of tibialis anterior can completely rupture.
This is more common in:
- men over the age of 70 years
- long-standing tendinopathy
- gout
- diabetes
- people having steroid tablets or tibialis anterior injections.
Interestingly, this event can be without injury (spontaneous). Mild transient pain occurs, a swelling
appears in front of the ankle (“pseudo-tumour”), and a foot-drop gait
develops. The toe extensor tendons are recruited to help lift the foot which can cause "clawing". Surgery is not always required (see below) and is more complex than just sewing the tendon ends together.
Laceration
by a falling knife or broken glass door is another cause of tibialis anterior rupture. This requires urgent surgery.
"Foot-drop" can also be due to nerve (spine, hip or knee level) or tibialis anterior muscle damage.
Interesting fact: poliomyelitis caused many cases of "foot-drop" due to tibialis anterior weakness (as well as severe paralysis and death) before routine vaccination was introduced to Australia in the 1950s. Immunisation works!
How are Tibialis Anterior Tendon Problems Diagnosed?
The diagnosis is usually clear after taking a complete history and performing a physical examination.
Investigations commonly arranged are:
- ultrasound and/or MRI scan of the foot
- weight-bearing X-rays of the foot looking for midfoot arthritis.
Sometimes an injection of local anaesthetic is used to confirm where the pain is really coming from.
How are Tendinopathy and Split Tears Treated?
Most people improve with non-surgical treatment unless a large split tear is present.
Non-surgical treatment
Non-surgical treatment involves:
- reduced activity on uneven ground
- anti-inflammatory medications
- supportive shoes and insoles
- physiotherapy
- cortisone injections.
Surgery for tibialis anterior tendinopathy and split tears
If symptoms are not improving
after several months of non-surgical treatment, or a large split tear
is present, surgery is often recommended.
The aim of surgery is to assist tendon healing and correct any associated condition. This always involves:
- tibialis anterior tendon exploration with "clean-out" (tenosynovectomy) +/- split repair.
Other possible procedures include:
- removal of bone spurs
- calf lengthening
- tibialis anterior reconstruction (see below).
A "moon-boot" is not usually required.
Full recovery takes at least six months and recurrence can occur (15%).
How is Tibialis Anterior Complete Rupture Treated?
People with complete rupture of this tendon fall into two groups:
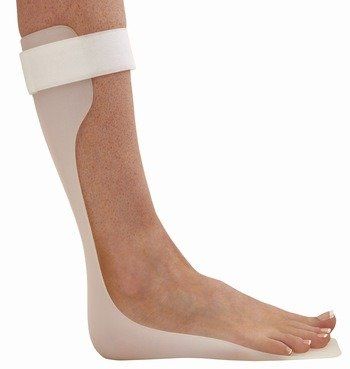
1) those that have health issues and low-demand:
- surgery is too risky
- non-surgical treatment is always recommended
- a Foot-Up brace or plastic splint (AFO) is fitted to prevent "foot-drop" and improve walking.
- deeper shoes prevent toe rubbing and also improve walking.
2) those that are
well and active:
- surgery involves tibialis anterior reconstruction (see recovery timetable below)
- this replaces the ruptured tendon with a gracilis graft (hamstring tendon) or the EHL tendon (big toe tendon)
- calf lengthening is often required at the same time.
Surgery:
- one or two night stay in hospital
- requires a general or spinal anaesthetic
- takes 60 - 90 minutes.
First 2 weeks:
- bandage
- "moon-boot" day and night
- crutches or frame
- rest, elevation and ice (RICE)
- gentle ankle movements
- post-operative appointment.
Next 4 weeks:
- "moon-boot" +/- crutches or frame
- physiotherapy-guided strengthening program
- RICE as needed.
Next 4 weeks:
- "moon-boot" to stand and walk only
- exercise bike and pool exercises.
Next 9 months:
- return of leg strength
- improving gait pattern.
Benefits and risks:
- 90% of people are helped by this surgery
- 2% of people are made worse by surgery.
Consequences and complications:
- no driving (4 to 10 weeks)
- re-rupture occurs in 5% of people
- thigh bruising is common if a hamstring used
- big toe drooping can occur if EHL used
- see General Information about Surgery.