Achilles Tendinopathy
What is Achilles Tendinopathy?
Achilles tendinopathy is a chronic condition that is more common with aging. It is a combination of inflammation (tendinitis) and "wear and tear" (degeneration).
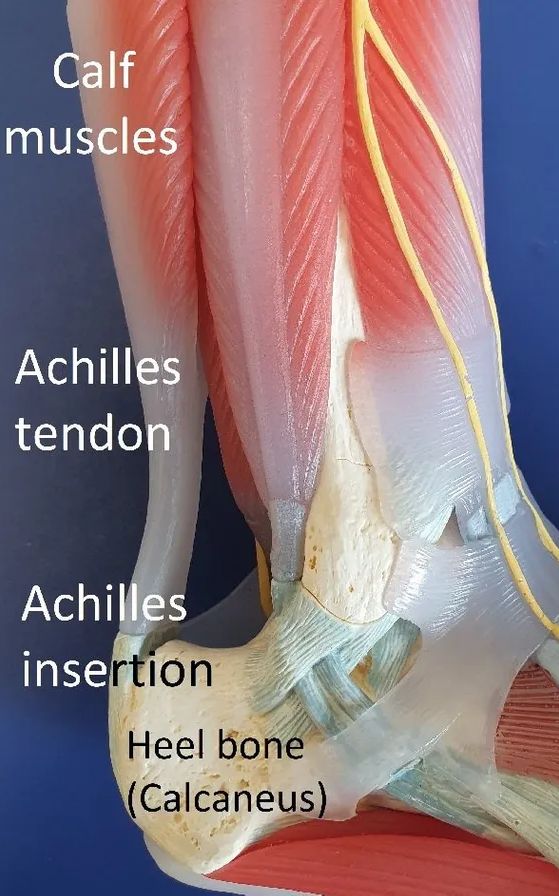
Two areas of the tendon can be involved:
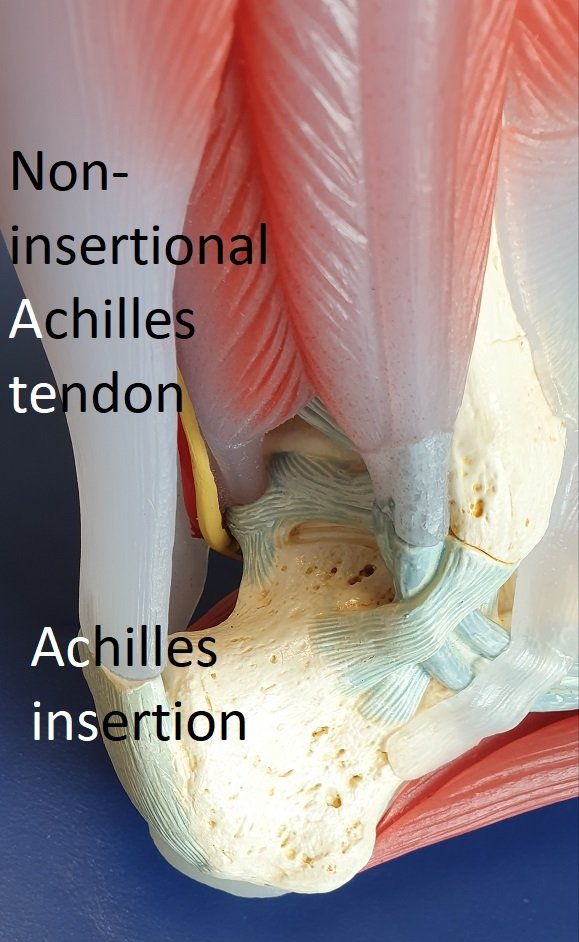
- non-insertional disease +/- paratenon and plantaris involvement
- insertional disease and spurs
What Causes Achilles Tendinopathy?
Achilles tendinopathy is the result of gradual accumulated "wear and tear" in the tendon from overuse or ageing. The tendon cannot heal itself well enough to keep up with the damage.
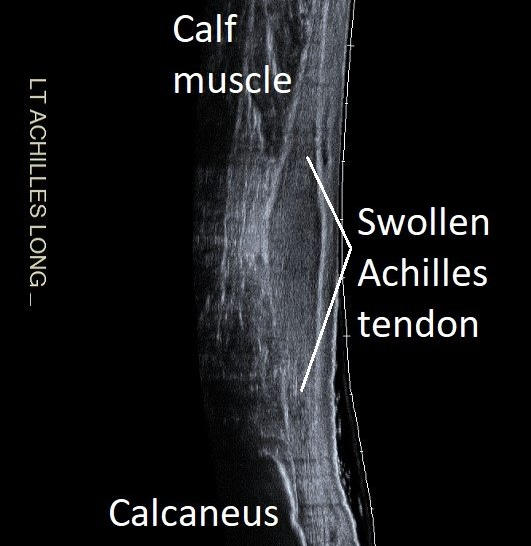
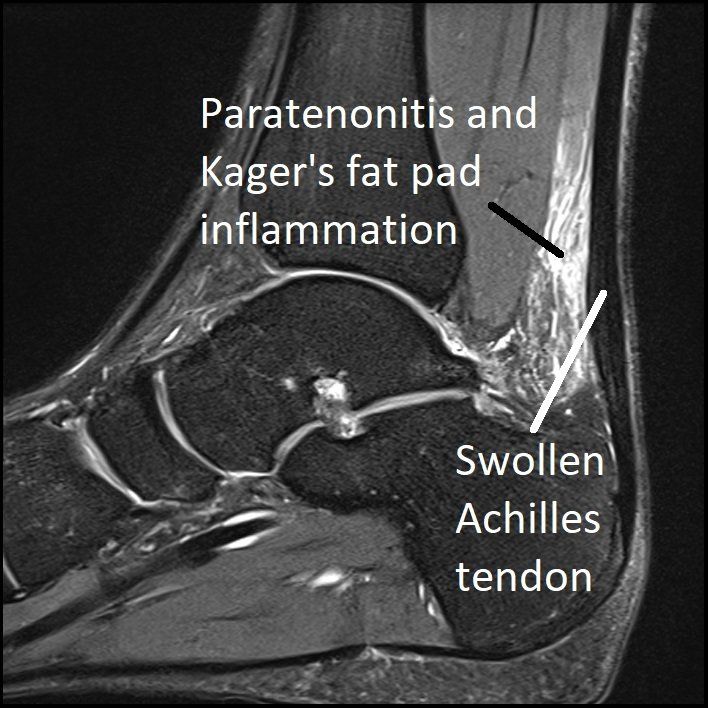
The tendon becomes thickened and painful. Splits can occur in the tendon.
Complete rupture is fortunately uncommon (see Achilles Tendon Rupture
in the ACHILLES & HEEL menu).
Common causes and associations include:
- over-training or unaccustomed use – “too much, too soon”
- change in training surface – e.g. grass to bitumen, or hill running/climbing
- lack of training variation
- poorly supportive footwear.
It is also more common in:
- gender: men > women
- age: > 30 years most common
- weight: higher body weight increases risk
- diabetes
- calf weakness, poor endurance or tightness
- stiff ankle and foot joints.
Achilles Non-insertional Tendinopathy
This is characterised by a painful, tender and swollen tendon 2 - 6cm
above
the insertion
(attachment) on to the heel bone. Morning and start-up stiffness are common. Pain often improves with "warming-up" but gets worse after prolonged activity.
Runners typically develop a reactive “tendinitis” triggered by increased training. This can return to a normal tendon with correct treatment. Modern research performed through the Australian Institute of Sport has identified a spectrum of disease severity and the role of paratenon and plantaris adhesions. (See Paratenonitis and Plantaris
in the ACHILLES & HEEL menu).
Older people typically present with degenerative softening, splits and
calcification of the tendon. This usually does not return to normal but symptoms can be improved by treatment.
Achilles Insertional Tendinopathy and Spurs
This form of the condition occurs at
the insertion
(attachment) of the Achilles tendon on to the heel bone (calcaneus). It is associated with aging, obesity and sero-negative inflammatory arthritis (psoriatic arthritis, ankylosing spondylitis, DISH, etc).
Pain and swelling are lower than in non-insertional tendinopathy. The back of the heel is often bulky and inflamed, making tight shoes uncomfortable to wear.
Most people also develop bony heel spurs
that grow up inside the tendon from the calcaneus (see images).
This condition is not the same as Haglund's syndrome or retrocalcaneal bursitis.
How is Achilles Tendinopathy Diagnosed?
Diagnosis is usually obvious after thorough history taking and clinical examination.
Imaging is useful when progress with physiotherapy is not occurring as expected or other forms of treatment are planned.
Lateral heel x-rays show insertion bone spurs. Ultrasound and MRI look closely at the tendon.
Non-surgical Treatment of Achilles Tendinopathy
Achilles tendinopathy treatment has improved significantly in recent years. Physiotherapy and other non-surgical treatments are used in all cases. Please see Non-surgical Treatment
in the TREATMENTS menu.
It can take weeks to months for recovery to occur. The longer the symptoms have been present, the longer healing will take.
Controlled Loading and Eccentric Strengthening.
Prolonged rest is not advised.
Gradually increasing Achilles load over several months is very important to recovery.
- Mild load increases stimulate tendon growth.
- Overload leads to tendinopathy deterioration.
When managing load you should be guided by how the tendon feels both immediately and also 24 hours later. It is important to modify activity to remain comfortable during and after loading.
Local Treatments.
These aim to reduce pain and swelling, and can help tendon healing.
- "Shockwave therapy" (ultrasound)
- Dry-needling.
- Anti-inflammatory gels.
- Shoes with small heel raises.
- high volume injections to "strip" the paratenon off the Achilles tendon
- PRP injections to stimulate healing of the tendon.
Please see Non-surgical Treatment in the TREATMENTS menu.
Surgical Treatment of Achilles Tendinopathy
Surgery is only recommended when non-surgical treatments have been tried for at least four to six months.
Non-insertional Achilles Tendinopathy.
In the past, surgery involved cutting out large amounts of the Achilles tendon, often requiring major reconstruction and recovery time. Today, it is rare for this to be required as less invasive procedures are just as effective.
- Paratenon and plantaris release
- TOPAZ radio-frequency stimulation.
Insertional Achilles Tendinopathy.
This condition is not as easy to treat by non-surgical methods, especially when a large heel spur is present. Surgery involves elevation of the Achilles from most of its insertion, removal of the spur and degenerate tendon, then reattachment to the heel bone with strong sutures.
Surgery requires six weeks walking in a "moon-boot" then rehabilitation. Final recovery can take six months or more. 90% of people are happy with the results of surgery after full healing.
See Achilles SpeedBridge
in the TREATMENTS menu for more information.