Non-surgical Treatment
Rest, Ice, Compression and Elevation
The best early treatment recommended after injuries and surgery is rest, ice, compression and elevation (RICE).
- Rest: limiting activity reduces pain, swelling and further damage. Crutches may be needed.
- Ice: an ice-pack should be used on the swollen area during the first three days. Never place ice directly on the skin.
- Compression: this is by using an elastic bandage for a few days or weeks.
- Elevation: having the ankle above your heart level reduces swelling and bruising. This is very important in the two weeks after injury/surgery.
Braces and "moon-boots" are used when the ankle or foot need to be immobilised.
Gentle movements are always encouraged to prevent stiffness and blood clots.
Medications
Oral medications
All medications have side-effects.
Always be aware of allergies.
Read the Patient Information provided with the medication.
If unsure, speak to your GP, specialist and Dr Beamond.
Analgesics - pain relieving medicines.
- Paracetamol: safe and useful alone for mild pain or in combination with others for strong pain. No more than eight tablets in 24 hours.
- Tramadol and Tapentadol (Palexia): stronger medications with side-effects.
- Codiene and oxycodone: strong medications that can cause addiction if taken for too long. See General Information about Surgery. These medications are not appropriate treatment for chronic pain is most people.
Anti-inflammatories - reduce pain and inflammation. Also called NSAIDS. Examples are ibuprofen, voltarin and meloxicam.
- Safe in most people but prolonged use is harmful. Have with food and do not consistently take every day.
- Do not take without medical advice if kidney problems, asthma, high blood pressure and/or GORD and peptic ulcer disease.
Complimentary medicines
- may help and can also have side-effects.
- Fish oil, krill oil, tumeric, etc: have anti-inflammatory properties.
- Glucosamine and chondroitin sulphate: may help symptoms of early osteo-arthritis.
Topical medications
Anti-inflammatory creams and gels - are very popular (and expensive).
- There is some evidence that they work in acute soft tissue injury (sprain and muscle tear).
- They do not penetrate further than a few millimeters under the skin.
- They can cause a skin rash if used too often. Sports Doctors may prescribe a "Voltarin wrap" under supervision.
- They should not be used on broken skin.
- Small amounts of the medication do enter the blood stream.
Cortisone injections - are commonly used to treat conditions of the foot and ankle.
- Cortisone and related medications have strong anti-inflammatory properties. They are corticosteroids related to prednisolone.
- They work best when inflammation is a major part of the problem and don't cure degeneration or osteo-arthritis.
- Local anaesthetic is mixed with the cortisone providing immediate but temporary pain relief in most people.
- The cortisone takes several days to weeks to work (if it is going to) and lasts weeks to months in some people.
- The injection is usually performed with ultrasound guidance.
- The risks are small, but pain can flare and infection occurs < 1 in 1000 cases.
- Evidence supports its use for ankle synovitis, peroneal tenosynovitis and sinus tarsi syndrome.
PRP injections
- are sometimes used to help tendons (Achilles tendinopathy, etc) and other soft tissue heal.
- Platelet rich plasma (PRP) is a concentrated fluid made from a person's own blood.
- Evidence varies as to if it works and in which conditions it helps most.
- Some people find the injections very painful despite local anaesthetic.
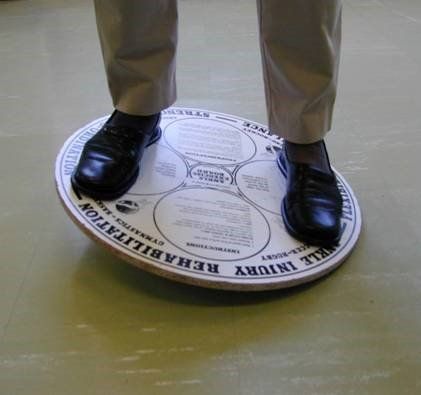
Physiotherapy
There are many possible treatments provided by a physiotherapist.
Most of the benefit comes from:
- swelling control after injury
- regaining joint movement
- muscle strengthening and tendon stretching
- regaining balance (proprioception).
Other treatments can improve pain and sensitivity. Examples are dry-needling and shockwave therapy (see below).
Your doctor and/or physiotherapist will work out which treatments are right for you and monitor progress.
Careful instructions to your physiotherapist are always provided after surgery.
It is important to continue exercises at home between visits.
Podiatry and Insoles/Orthotics
What are orthotics?
Orthotics:
- are better known as insoles. However, there are other types of orthotics such as splints and braces (see below).
- can be modified or even custom-made to fit a person's feet.
- hard orthotics are only appropriate in flexible "young" feet, not stiff arthritic feet. Most people find semi-rigid orthotics more comfortable.
Some conditions benefit from custom orthotics. Unstable high-arched feet and painful flat feet are two examples.
Other conditions just need supportive shoes and insoles from a chemist or shoe shop (plantar fasciitis in most people).
Other podiatric treatments
Apart from orthotics, podiatrists are valuable in providing:
- education on foot structure and general care
- advice on shoes and activities. Some specialise in running, dance, heel pain, etc
- foot taping and strengthening exercises
- nail and skin care. All people with diabetes should have a podiatrist
- shockwave therapy (see below).
Splints and Braces
These devices help control movement and give stability to the ankle and hindfoot joints.
Common types are:
- lace-up or velcro ankle brace. Also called an ASO (ankle stabilising orthosis)
- "moon-boot". Also called a CAM boot (controlled ankle motion boot)
- night splints and Strassburg sock (used occasionally in plantar fasciitis)
- thermoplastic splint. Also called an AFO (ankle foot orthosis).
Shockwave Therapy
What Is shockwave therapy?
Shockwave therapy is a non-surgical treatment for soft tissue pain, inflammation and degeneration.
It involves:
- the delivery of high-frequency sound waves to the injured tissue to stimulate healing
- there are several types of shockwave therapy. The science continues to advance.
- most people have it provided by a hand-held probe, such as a Dolorclast-type device.
The full name for this treatment is extracorporeal shockwave therapy (ESWT).
Interesting fact: one of the earliest uses of ESWT was to break-up kidney stones.
What conditions can be treated using shockwave therapy?
Shockwave therapy is a methods used to treat chronic tendon and soft tissue conditions including:
70% of people have some benefit from this treatment. Several sessions are required and final improvement can take six months.
Side effects:
- temporary redness, pain and swelling at the site of treatment
- the safety of shockwave therapy has not been evaluated in pregnant women and children, and should not be used on them.
What does shockwave therapy involve?
Shockwave therapy is usually administered by a podiatrist, physiotherapist or sports doctor.
A session involves the following steps:
- the target area is located, marked and ultrasound gel applied
- sometimes local anaesthetic is also used
- the hand-held probe is held lightly on the skin
- sound waves are given as short pulses of less than 1 microsecond, with 1000 to 4000 pulses given
- the treatment can take between 5 to 30 minutes.
After a session:
- people are able to go home immediately
- mild pain relief medication may be needed
- return to work and normal activities are possible within one or two days after the therapy.
The number and intensity of the sound waves will depend on the severity of the condition.
Treatment may require two to five sessions of therapy at weekly intervals.