5th Metatarsal Fracture
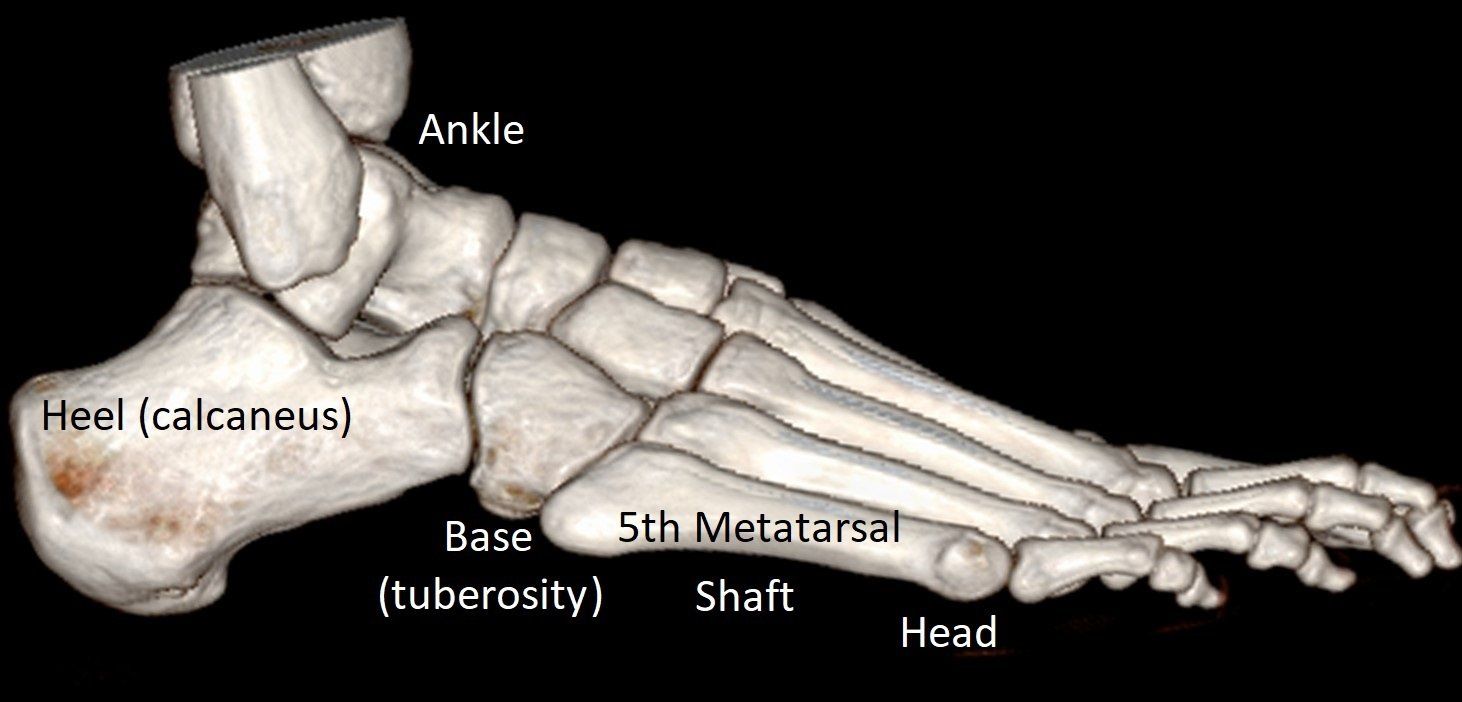
What is the 5th Metatarsal Bone?
The 5th metatarsal bone is the long bone located on the outside of the foot.
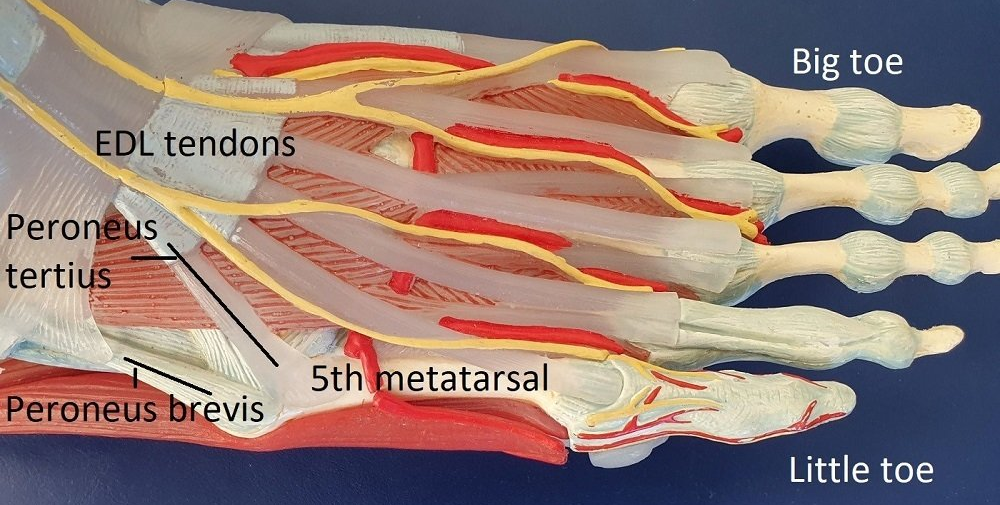
It has a base (tuberosity) where the peroneus brevis tendon and lateral plantar fascia attach, a long shaft and a head where it meets the 5th toe.
Please see Foot - Anatomy and Imaging for more information on where this bone is in the foot.
Types of 5th Metatarsal Fracture
- There are several types of 5th metatarsal fracture.
- They usually occur due to twisting injury.
- Most heal without complication but can take time.
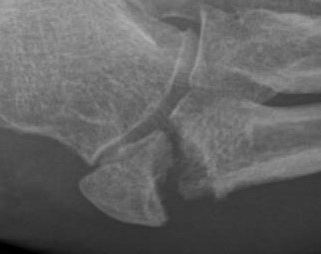
Base (Tuberosity) Avulsion Fracture
- In an avulsion fracture, a piece of the bone is pulled off the main portion of the fifth metatarsal by the attaching plantar fascia or tendon.
- These are the most common 5th metatarsal fracture.
- They are a cause of persisting pain after what is thought to be an ankle sprain.
- Treatment is protection in a stiff sole shoe or low "moon-boot" until comfortable.
- Surgery is rarely required, unless the avulsed fragment is very displaced and not healing (see images below).
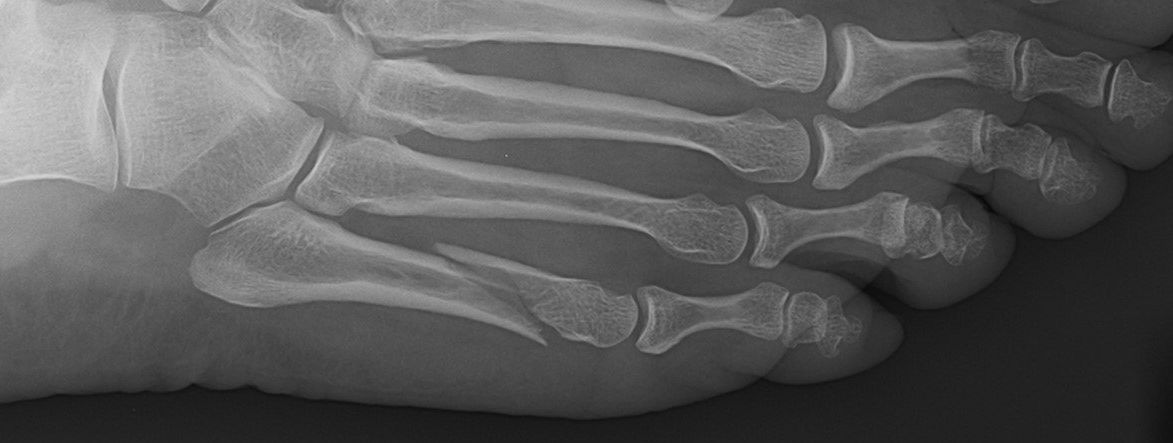
Shaft, Head and Neck Fractures
- Neck and head fractures (uncommon).
- Shaft fracture ("dancer's fracture") - these spiral fractures look bad but heal without surgery (see images below). Surgery can actually make them heal slower.
Jones Fracture
- This fracture occurs in an area between the base and shaft of the fifth metatarsal which has a limited blood supply and is under tension stress on standing (see image).
- This injury heals slower than a base avulsion fracture. It sometimes does not heal or re-fractures after healing. Surgery may be recommended early in active people.
Stress Fracture of the 5th Metatarsal
- This stress fracture of the foot occurs in a similar location to the Jones fracture but develops over time rather than acutely from an injury (see image - note thicker "whiter" bone).
- People with high arched (cavo-varus and metatarsus adductus) feet are more likely to have this stress fracture.
- Healing is slow and re-fracture can occur. Surgery is usually recommended.
5th Metatarsal Jones and Stress Fracture - symptoms
- pain,
- swelling,
- tenderness,
- and bruising over the outer foot.
- Difficulty walking.
5th Metatarsal Jones and Stress Fracture - diagnosis
- history of injury
- examination of the foot.
5th Metatarsal Jones and Stress Fracture - treatment
- rest, ice, compression, and elevation (RICE) to help control pain and swelling
- a splint or "moon-boot"
- crutches to keep weight off the foot.
Surgical Treatment of 5th Metatarsal Jones and Stress Fractures
- Jones fracture surgery is recommended when the fracture is not healing well or re-fracture occurs, and in active people or high-risk feet.
- Stress fractures of the 5th metatarsal usually require surgery.
Interesting fact: Dr Beamond has fixed these fractures in members of the Adelaide Crows, Adelaide 36ers and Adelaide United clubs.
Surgery involves placing a screw within the 5th metatarsal to stabilise the bone and allow the fracture to heal (see images below). Occasionally a metal plate is required instead.
Bone graft is used when needed to stimulate healing.
Surgery:
- is often Day Surgery
- requires a general anaesthetic in most people
- takes 30 minutes.
First 2 weeks:
- bandage
- "moon-boot" and crutches
- rest, elevation and ice (RICE)
- ankle and foot movements
- post-operative appointment.
Next 4 weeks:
- "moon-boot" to stand and walk
- exercise bike and pool-based activities
- post-operative appointment and X-ray.
Next 1 to 2 months:
- shoes
- return to sports specific training then sport
- post-operative appointment +/- X-ray.
Benefits and risks:
- 95% of people are helped by surgery
- 5% of people need more surgery
- <1% of people are made worse by surgery.
Consequences and complications:
- driving restrictions (2 to 8 weeks)
- scar numbness is common
- re-fracture if return to sport before 10 weeks
- screw or plate is NOT normally removed
- see General Information about Surgery.